In a time of unprecedented transformation in the healthcare industry, staying informed and inspired is not just a benefit — it’s a necessity. That’s why Elligint Health is proud to bring you Sparking Change, our monthly e-newsletter designed especially for our clients and partners. More than just an update, Sparking Change is your strategic companion — offering insights into innovation, performance, and the people driving progress across healthcare.
Where to Begin: Three Care Management Programs that Deliver Early Value in Value-Based Care
Starting a care management program from scratch can feel overwhelming. With limited resources and pressure to show return on investment (ROI) quickly, it’s essential to focus on programs that are both high-impact and sustainable. These three CMS-supported initiatives offer a powerful combination of revenue potential, outcome improvement, and scalability for new care management teams.
1. Chronic Care Management (CCM)
CCM supports patients with two or more chronic conditions through regular care coordination outside of in-person visits. This includes monthly check-ins, medication monitoring, and help with self-management.
Why start here: CCM targets patients at high risk of hospitalizations and ER visits. It also builds the foundation for deeper patient engagement and long-term cost control.
Key Benefits:
• Proactively manages high-risk and potentially high-cost patients
• Reduces utilization through consistent outreach
CMS Reference
2. Transitional Care Management (TCM)
TCM helps patients safely transition home after a hospital or skilled nursing facility stay. It reimburses for follow-up care coordination, including prompt outreach and a timely office visit.
Why start here: The immediate post-discharge period is one of the highest risk times for complications. TCM reduces readmissions and improves patient outcomes while generating revenue for a service most practices already perform.
Key Benefits:
• Prevents high-cost readmissions
• Strengthens care continuity after hospitalization
CMS Reference
3. Behavioral Health Integration (BHI)
BHI brings mental health support into primary care by reimbursing for collaborative care of conditions like depression and anxiety. A team approach that includes a primary care provider, behavioral health manager, and psychiatric consultant helps deliver more holistic care.
Why start here: Mental health concerns often complicate chronic disease management and increase costs. Addressing them early improves adherence, engagement, and overall health outcomes.
Key Benefits:
• Tackles an often-overlooked driver of cost
• Supports whole-person care and improves chronic care management and patient experience
CMS Reference
Start Small, Think Big
Starting with CCM, TCM, and BHI gives organizations a strategic basis that can improve outcomes, enhance patient relationships, and create financial sustainability. These foundational services represent practical, proven paths for new care management teams to deliver better care, drive early ROI, and prepare for more advanced population health strategies in the future.
Team Spotlight: Rebecca Vos, Vice President of Client Business Solutions
In her role as Vice President of Client Business Solutions at Elligint Health, Rebecca Vos serves as a trusted partner to our clients — building strong, collaborative relationships and ensuring their success with our Helios® suite of products and integrated partner applications. By taking the time to deeply understand each client’s unique business goals and operational challenges, Rebecca delivers tailored solutions that help our customers maximize value, streamline services, and deliver better outcomes.

Rebecca began her career working as a project manager in residential construction followed by software project management & training in the provider space. Motivated by her desire to make a greater impact, she returned to school at the University of Texas at Dallas to pursue her passion for healthcare. She subsequently launched her healthcare career at Health Care Services Corporation (HCSC) in Clinical Operations supporting both Commercial and Government programs. During this time, she played a pivotal role in implementing Texas Medicaid’s first Long Term Services and Supports (LTSS) program, helping to shape the program by using her deep operational and clinical insights. She also served as a Senior Project Coordinator across several Blue Cross and Blue Shield plans, including Illinois, Montana, New Mexico, Oklahoma, and Texas.
Over the past seven years Rebecca has continued to apply her clinical and operational expertise to guide successful client implementations and long-term strategies.
“As a team, our greatest achievements happen when our clients succeed,” Rebecca says. “I’m passionate about understanding their goals, helping them navigate our solutions with confidence, and building partnerships that last. My mission is to ensure every client feels heard, supported, and empowered to deliver exceptional care.”
Solution News You Can Use
Insights, updates, and helpful tips from your team at Elligint Health
Check Out the New Elligint Health Website: Did you know that we have a new website? Visit https://elliginthealth.com/ to get the latest product news, read recent blog posts and newsletters, and learn how Elligint Health is growing to better serve the needs of our customers. For current clients trying to access training videos, please contact your Account Manager to get updated access to learning resources.
Coming Soon to a Platform Near You: Get ready for the rollout for Utilization Management (UM) 3.0! Our next-generation UM solution will feature several new technologies to help organizations meet the new CMS-0057-F Interoperability and Prior Authorization Final Rule. New tools such as Quick Navigation to facilitate movement through complex forms, Attention Guidance to help highlight what matters most in UM processing, Quick Entries that enable bulk actions that accelerate efficiency, and Quick References that provide contextual information via innovative side panels help to streamline workflow and deliver more timely and effective care. Elligint Health will be rolling out these enhancements this fall with a webinar as well as client-specific training. To find out more, contact your Account Manager today.
Did You Know? Helios® comes with an industry-leading Assessment Builder that provides users with unparalleled flexibility and power in customizing existing assessments and creating new ones. The builder provides an intuitive and easy-to-use visual wizard that allows administrators to create virtually any type of question (e.g., date, time, number, free text, table, drop-down, radio button, checkbox, signature, etc.); create custom branching, mapping, workflows, and scoring rules; and adjust layout and design.
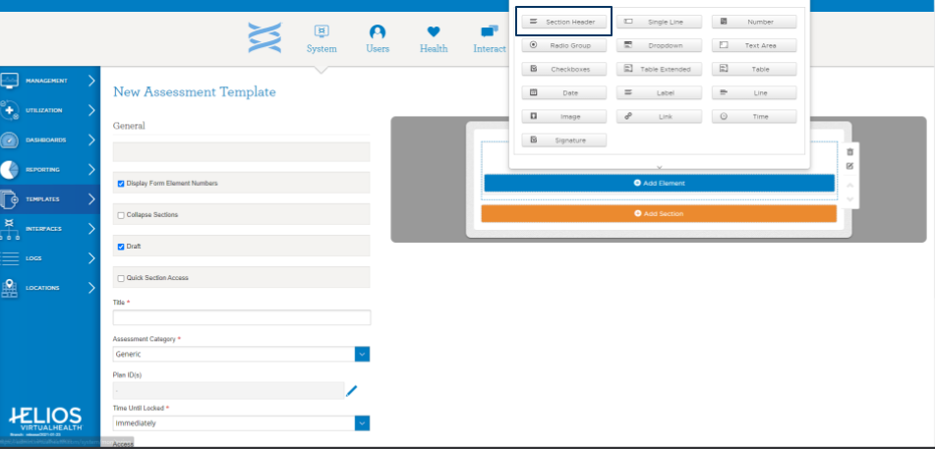
To find out more about building and modifying templates and how they can make your workflows more efficient, contact your Account Manager.
How Does the Provider Portal Differ from the Care Manager Portal? The Provider Portal and the Care Manager Portal are designed to cater to different user needs within Helios. The Provider Portal is tailored to meet provider-specific needs, offering features such as authorization request submission, claims status, appointment management, referrals, formulary lists, and encounter notes. It allows providers to have visibility into medical management activities, review tasks, participate in communication with care team members, and send referrals for care management services. On the other hand, the Care Manager Portal is part of the integrated system that blends administrative, care manager, provider, patient, and caregiver/family portals, providing comprehensive functionality across care management (CM), disease management (DM), and utilization management (UM). The Care Manager Portal is likely more focused on the coordination and management of care activities, while the Provider Portal is more focused on provider-specific administrative and clinical tasks.
Groundbreaking Collaboration Among Health Insurers Aims to Simplify Prior Authorization Process
Nearly 50 major U.S. health insurers — including Aetna, Blue Cross Blue Shield companies, Cigna, Himark, Humana, Kaiser Permanente, and UnitedHealthcare — have voluntarily committed to a set of reforms aimed at streamlining the prior authorization process. These reforms include reducing the volume of medical services that require prior authorization, improving transparency around denials and appeals, and adopting a standardized electronic system by 2027. Other elements of the pledge involve ensuring continuity of prior authorizations during insurance transitions and committing to faster decision times, with a goal of handling at least 80% of approvals in real time.
The planned reforms, which meet and exceed those contained in CMS’s Interoperability and Prior Authorization Final Rules (CMS-0057-F), will be implemented across commercial, Medicare Advantage, and managed Medicaid plans covering approximately 257 million Americans. Industry reaction has been uniformly positive so far, with stakeholders across the healthcare landscape viewing the reforms as a necessary step toward reducing administrative burden on providers and improving patient access to timely care.
Helios® UM by Elligint Health empowers payers to meet the demands of CMS-0057-F and insurer-led reform initiatives with confidence. By combining robust automation, FHIR-enabled APIs, real-time data sharing, and comprehensive prior authorization tracking — all within a unified, user-friendly interface — Helios UM streamlines utilization management, improves decision accuracy, and accelerates processing times.
Sources
https://www.beckershospitalreview.com/finance/insurers-pledge-ease-to-prior-authorizations/
https://www.cnbc.com/2025/06/23/prior-authorizations-us-insurers-to-change-approval-process.html
https://www.ahip.org/health-plans-are-making-voluntary-commitments-to-support-patients-and-providers
https://www.bcbs.com/news-and-insights/article/right-care-right-place-right-time
For more information about Elligint Health, contact your Account Manager today.


